The findings suggest that boosting signals in certain cells and not in others might even help treat colon cancer
Treating inflammatory diseases of the bowel is extremely challenging because their causes are complex: Genes, gut microbes and disrupted immune function are but some of the contributing factors. Weizmann Institute of Science researchers are proposing a way around this complexity. In a study in mice, published in Cell Reports, they have found a way to trigger a natural defense mechanism that prompts the body itself to alleviate intestinal inflammation.
The study, led by veterinarian Dr. Noa Stettner, who is also a PhD student in the lab of Dr. Ayelet Erez in the Biological Regulation Department, focused on nitric oxide (NO), a signaling molecule involved in a variety of biological processes. Scientists have long tried to determine what role NO plays in such inflammatory conditions as Crohn’s disease and ulcerative colitis, and whether it can be used in therapy, but studies failed to produce conclusive results: NO alleviated intestinal inflammation in some circumstances, but promoted it in others.
Different effects on different cells
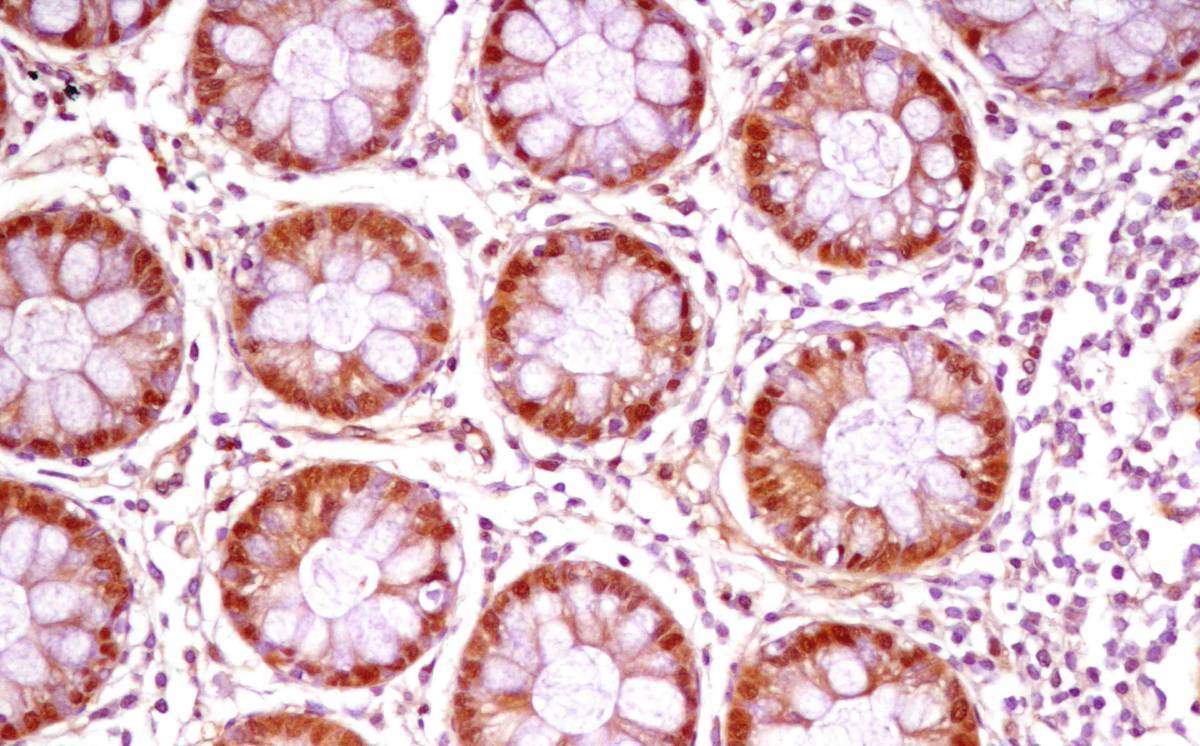
The Weizmann researchers hypothesized that the paradoxical findings might arise because NO has different effects in different types of cell in the gut. To test this idea, they genetically engineered mice to block NO production exclusively in certain types of cells: either in the cells making up the inner lining of the gut or in immune cells. They found that the symptoms of a colitis-like disease got worse when NO synthesis was blocked in the gut cells; in contrast, symptoms improved when NO was blocked in immune cells, particularly in large cells called macrophages. These results suggest that NO reduces inflammation when manufactured in the gut cells but increases inflammation when secreted by immune cells.
The scientists concluded that inflammatory bowel diseases may be treated by raising NO levels exclusively in the cells of the inner lining; yet if patients take NO directly as a drug, it may cause side effects in cells outside the gut lining. Stettner, with the help of collaborators at the Weizmann Institute and elsewhere, set out to develop a method for boosting NO production only in the gut lining cells.
The raw materials for NO production
They relied on Erez’s earlier finding that an enzyme called ASL plays a key role in NO production: It is responsible for the making of the amino acid arginine, the raw material from which the body manufactures NO. The researchers decided to jump-start this mechanism. They made use of two natural substances: One was fisetin, which is present in apples, persimmons, strawberries, and other fruits and vegetables, which they found to elevate ASL levels; the other was citrulline, found in watermelon, beets, spinach and other plants, which increases ASL activity.
“Our hope was that if we prompted the organism to make ASL and strengthen its activity, it would in turn manufacture NO only where it’s needed and not where it can do harm,” Stettner says.
The approach worked: The two supplements, when given together, promoted the manufacture of NO exclusively in cells of the inner lining of the gut. Most important, in mice treated with these two supplements, symptoms of an inflammatory disease in the gut improved significantly.
Moreover, the treatment had a beneficial effect on colon cancer, which is known to be aggravated by severe inflammation of the gut. When the researchers gave the two supplements to mice with tumors of the colon, not only did their intestinal inflammation subside, but their tumors decreased in number and size.
The two supplements, together, promoted the manufacture of NO exclusively in cells of the inner lining of the gut
“We trusted the body to make use of its own healing mechanisms,” Stettner says. “We provided it with the building blocks and let it manufacture NO in the right amount and exactly in the right place.”
If this approach is shown to raise NO levels in the inner lining cells in humans, it may help treat inflammatory bowel diseases − and potentially perhaps even decrease the complications of colon cancer. The fact that it makes use of substances available as over-the-counter nutritional supplements should facilitate its implementation.
Contributors to this research included: Julia Frug, Dr. Alon Silberman, Dr. Alona Sarver and Dr. Narin N. Carmel-Neiderman of the Biological Regulation Department; Dr. Chava Rosen, Dr. Biana Bernshtein, Dr. Shiri Gur- Cohen, Dr. Meirav Pevsner-Fischer, Dr. Niv Zmora and Prof. Steffen Jung of the Immunology Department; Dr. Raya Eilam, Dr. Inbal Biton and Prof. Alon Harmelin of the Veterinary Resources Department; Dr. Alexander Brandis of the Life Sciences Core Facilities Department; Dr. Keren Bahar Halpern of the Molecular Cell Biology Department; Dr. Ram Mazkereth of Tel Aviv University; Dr. Diego di Bernardo and Dr. Nicola Brunetti-Pierri of Federico II University in Naples, Italy; Dr. Gillian Dank of the Hebrew University of Jerusalem; and Dr. Murali Premkumar and Dr. Sandesh CS. Nagamani of Baylor College of Medicine in Houston, Texas.
Dr. Ayelet Erez’s research is supported by the Adelis Foundation; the Rising Tide Foundation; the Comisaroff Family Trust; the Irving B. Harris Fund for New Directions in Brain Research; and the European Research Council. Dr. Erez is the incumbent of the Leah Omenn Career Development Chair.
Recent Comments